by Jenny Yang (CHEERI Medical Student Representative)
Dr Hannah Mechie is a ST7 PEM SPIN registrar, currently working on PICU at Addenbrooke’s Hospital, Cambridge. She recently took part in a Quality Improvement Project (QIP) training course run by Improve ONE Thing, and it has completely changed her understanding of running QIPs to truly make a difference to patients, and she passionately recommends this course to everyone.
What is the Improve ONE Thing QIP course?

This is an online course run by QIC Learn Improve ONE Thing, which, over 16 weeks, takes you through the process of conducting a QIP using the Model of Improvement. Once we had learnt about the basics of how to do a QI, we had to identify a project we would be motivated to conduct, and we were taken through the process of running this QIP for the rest of this course.
All the attendees were paediatricians (QIC Learn run courses specific to different specialties) at all stages of training – from ST2 to consultant level. So it’s never too late to learn how to do QIPs!
What are the key points you learnt about conducting QIPs from this course?
- Start small – it’s not really realistic to make extravagant changes to completely transform patient care in a short timeframe, so it’s important to find the small things which could have an impact and expand from there.
- Really, really assess the problem – try and work out the process and exactly what happens – the fishbone model is really helpful for this!
This approach makes running QIPs quite different to the large scale audits, which involve a big analysis with big recommendations to be presented at an audit meeting. Instead, there is a clear focus on identifying a problem and trying to solve it through small iterations.
What was your project as part of the QIP course? How much of an impact did this make?
The overview of my project was on streamlining the management of suspected neonatal sepsis. There are often delays in the process for babies with risk factors for neonatal sepsis who are actually clinically stable. In particular, waiting for the neonate’s blood culture to come back negative, can lead to unnecessary additional overnight stays before being discharged. I assessed each step in the process, and analysed what different problems could arise in each step (using the fishbone model), to create a list of ideas of what could be changed to improve this process. I also performed a cost analysis for the overnight stays, which was found to be £100,000 a year in wasted hospital admissions!
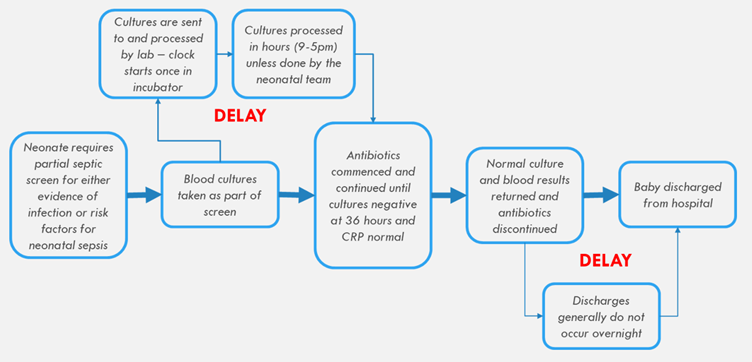
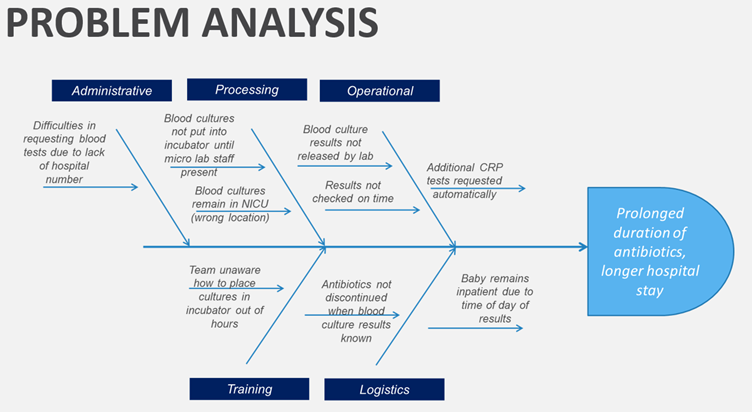
One of the reasons for delay in culture which I identified was that 50% of the trainees didn’t know where the incubator was, let alone how to use it, which is what we’re meant to do with blood cultures when out-of-hours. Therefore, one action point included making a map to direct people to it, leading a teaching session, and organising a little competition for who could do it most quickly! This was found to drastically reduce the time for getting blood culture results. With this strong evidence, I also spoke at the new trainees induction about the importance of this for their future practice.
Now that my suggested action points have been implemented, it has been interesting to talk to people from other hospitals who do this process quite differently, so it would be interesting to assess the differences and perhaps considering changing the process entirely!
Why would you recommend this QIP course? Who would you recommend it to?
It’s such a shame that this course isn’t more widely known, and I really really enthusiastically encourage trainees of all stages, from ST2 to consultant level, to take part.
Whilst it does take some time commitment, as you’re working on a project that you’re interested in, your self-motivation is really important and at the end of the day, and you can really make a difference to clinical care.
I’m also really excited to present a poster of my work at the BMJ International Forum in Copenhagen in May.
In the meantime, if you’re interested in learning more about QIPs, or joining the QIC Learn course, you can find out more here:
- The Model for Improvement framework: https://qi.elft.nhs.uk/resource/the-model-for-improvement/
- The NHS guide to QIPs – the PDSA (Plan, Do, Study, Act) cycle and the Model for Improvement: https://www.england.nhs.uk/wp-content/uploads/2022/01/qsir-pdsa-cycles-model-for-improvement.pdf
- Improve ONE thing:The Full QIPOPEN Course Spring 2023 – QIClearn